Abstract
Functional three-dimensional skeletal muscle constructs (myooids) were engineered from myogenic cells harvested from the muscles of adult and aged rats. Myooids formed by self-organization of myogenic cells in the absence of an artificial scaffold and were maintained in culture. Myooid excitability and contractility were measured at days 1, 3, 7, and 24 after myooid formation. Skeletal muscle myosin heavy chain (MHC) content was measured and MHC isoforms were separated on SDS-PAGE gels and quantified. Adult and aged rat myooids had only ~35-60% of the skeletal muscle MHC content of control skeletal muscle from rats, the remaining MHC content consisting of isoforms found in cultured fibroblasts but not in control skeletal muscle. In addition, myooids expressed only developmental isoforms of skeletal muscle MHC, known to generate less specific force than adult isoforms. Myooids from aged rats generated greater normalized force than myooids from adult rats, but only 1-3% of that for adult skeletal muscle controls. Normalizing for skeletal muscle MHC content and isoform expression predicts myooid forces of ~6-18% of control adult skeletal muscles. We hypothesize that the remaining force deficit is due to cellular and sub-cellular disorganization—Myooids lack the density and organization of sarcomeric arrays seen in skeletal muscle.
Introduction
One of the great advantages of tissue engineering of skeletal muscle is that adult skeletal muscle contains many myogenic precursor stem cells, termed “satellite cells”, which are involved in the repair and regeneration of skeletal muscle throughout the lifespan. Satellite cells are in general easy to isolate from explanted skeletal muscle, and presumably muscle biopsies from an adult mammal would provide an ample supply of cells committed to the myogenic developmental pathway to facilitate the in vitro engineering of functional skeletal muscle. With aging beyond adulthood, the pool of available satellite cells is known to decline [1-4]. Prior to tissue engineering of functional skeletal muscle from satellite cells harvested from aged mammals, two key questions must be addressed. First, to what extent are the satellite cells from aged mammals capable of fusion into functional myotubes, and second, do satellite cells from aged mammals have any form of impaired function when compared with those from young or adult mammals?
To study the capacity of satellite cells to form into functional skeletal muscle tissue de novo in culture, we have developed several in vitro tissue models. Functional skeletal muscle constructs termed myooids were previously tissue engineered in vitro by primary co-culture of myoblasts and fibroblasts from soleus muscles of adult rats [5-7] , mice and cell lines [6], and neonatal rats [7]. Myooids were activated by transverse electrical fields in a manner similar to that used to activate whole skeletal muscles in vitro during standard physiological measures of muscle function [8]. The myooids generated specific forces of ~0.1-3% of skeletal muscle from control adult rats. During a time course experiment, the contractile properties of adult rat myooids did not change over a period of several months in culture [7]. In contrast, the neonatal rat myooids initially had lower normalized force output than the adult rat myooids, but increased with time in culture up to ~2 months, at which time normalized force output of the myooids did not differ.
The purpose of the current study was to compare the excitability and contractility of myooids engineered from skeletal muscles of 32-month-old rats with that of myooids engineered from adult rat tissue. These aged male rats constitute only the surviving 15% of the original cohort of Wistar rats, and for the purposes of aging research are considered equivalent to human beings of ~90 years of age or older (US Dept. of Health and Human Services, Vital Statistics of the United States, 1994). Compared with control values from adult rats, aged rats have an extensor digitorum longus (EDL) muscle mass of 61%, and a maximum specific tetanic force (sPo) of 54%. Because of the decreased proliferation potential [9] and lower absolute number of satellite cells in muscles from the aged rats compared with adult rats [1,10,11], one may hypothesize that the aged rats would not yield enough myoblasts to produce myooids in culture. On the other hand, despite the atrophy and reduced myogenic potential of the EDL muscles in old rats, when an EDL muscle is cross-age transplanted from an old donor rat into a young host rat, the muscle regenerates as much mass and has as high a capacity for force development as a young muscle transplanted into a young host [4]. This suggests that the myogenic precursor cells from the aged rats may self-organize into myooids in culture as well as myogenic precursor cells from adult rats.
Therefore, the purposes of the current study were to: 1) culture myooids from muscles of adult and aged rats, 2) measure the excitability, contractile properties, and myosin heavy chain (MHC) composition of the myooids over their “lifetime” in culture, and 3) compare the excitability, contractile properties, and MHC content of the myooids from the muscles of aged rats with those of myooids developed from muscles of adult rats. Two specific hypotheses were tested: 1) the excitability and contractility of adult and aged rat myooids are not different, and 2) myooids contain less skeletal muscle MHC per unit mass than do control skeletal muscles.
Methods
The methods used for engineering myooids for this study are described in detail elsewhere [5,8,12] and are briefly given here. Rats were kept according to guidelines established in the United States Public Health Service Guide for the Care of Laboratory Animals (NIH Publication 85-23) and with the approval of the University (of Michigan) Committee on the Use and Care of Animals. Myogenic cells were harvested from the soleus muscles of one adult male Wistar rat (aged 5-6 months) and one aged male Wistar rat (aged 32 months) and cultured on laminin-coated SYLGARD substrates in 35 mm culture dishes. Cell cultures resulted in 40 myooids from the adult rat and 32 myooids from the aged rat used in this study, the difference in number being because of the greater mass of muscle tissue from the adult rat relative to the aged rat.
Culture media, dissociation solution, pre-incubation medium, culture plates, and silk suture anchors were prepared as described[5-8,12,14]. Growth Medium was F-12 Nutrient Mixture (GibcoBRL #11765-054) with 20% fetal bovine serum (GibcoBRL #10437-036) and 100 u/ml Penicillin G (SIGMA #P-3414). Differentiation medium was DMEM (GibcoBRL #11995-065) with 7% horse serum (GibcoBRL #16050-114) and 100 u/ml Penicillin G. Tissues were dissociated with a solution of 4 u/ml dispase (GibcoBRL #17105-041) and 100 u/ml type IV collagenase (Worthington #CLS 4) in DMEM. Each 35mm culture dish had a SYLGARD substrate that was coated with ~1 µg natural mouse laminin (GibcoBRL #23017-015)/cm2. Silk suture (#0 Ethicon) anchor points served as artificial tendons for the formation of myooids. One end of each 6 mm-long piece of silk suture was frayed and coated with laminin (50 g natural mouse laminin/ml in DPBS), and pinned into place in the culture dish with 0.1 mm minutien pins. Two silk suture anchor points were pinned in each culture dish in a straight line with 12 mm separating them at their closest points. Culture plates were placed in the incubator, each containing 2 ml of growth medium, for one week prior to plating of myogenic precursor cells.
Myogenic precursor cells were harvested from the soleus muscles of one adult and one aged rat by surgical removal of both whole soleus muscles. Each rat soleus muscle was sliced into 6 strips longitudinally from tendon to tendon, and pre-incubated (37C and 5 % CO2) in a solution of 90% differentiation medium, 10% isotonic saline and 0.005% NaN3 for 48 hours. Pre-incubation for 48 hours before enzymatic release of cells and plating in culture dishes resulted in maximal numbers of myoblasts as measured by time to confluence of culture plates(8).
After pre-incubation, muscle strips were enzymatically dissociated to release cells for primary culture by digestion in dissociation medium for 3 hours at 37C. Dissociated tissue was centrifuged (1200 g for 15 min) and resuspended in growth medium for plating. In preliminary experiments the optimal plating density for adult rat and aged rat myogenic precursor cells, as determined by minimum time to confluence, was found to be ~ 1 mg dissociated tissue/cm2 for adult rats and ~ 0.5 mg dissociated tissue/cm2 for aged rats. These plating densities were used in this study, allowing for the plating of 45 culture plates for adult rat myooids and 35 culture plates for aged rat myooids. Growth medium was changed 3 times per week until the cells reached confluence, when growth medium was replaced with differentiation medium, also changed 3 times per week. Myoblasts proliferated and fused to form multinucleated myotubes soon after cultures reached confluence. Myotubes began spontaneous contractions that eventually led to the delamination of the monolayer of cells. The monolayer detached from the substrate but remained attached to the silk suture anchors which acted as artificial tendons, and subsequently remodeled into a cylinder-like construct that was held in tension between the two artificial tendons above the substrate.
Contractile properties of each myooid were determined with an optical force transducer specifically designed for the task [8,13,14]. The force transducer was calibrated using a force generator of our design [13,15]. Myooid stimulation and collection of force data were carried out by use of a LabVIEW Virtual Instrument of our design [13]. During evaluation of contractile properties, myooids were maintained at 37 + 1 C by use of a closed-loop temperature controller.
At 1, 3, 7, 24, and 38 days after myooid formation for adult and aged rat myooids, groups of n = 8 myooids were removed from the incubator and subjected to contractile function tests in vitro. Since the optimum length for myooid force generation occurs at ~95% of culture length(8), before evaluation all myooids were shortened by 5% (0.6 mm) from the length at which they were cultured.
Myooid diameter, total cross sectional area (CSA), baseline force (Pb) which is also the resting tension generated by the myooid, peak twitch force (Pt), rheobase (R50), chronaxie (C50), and peak isometric force (Po) were determined as described in detail [5,8]. Specific Po was calculated by dividing Po by the CSA of the myooid. The authors recognize that more precise normalization would have been possible if CSA had been determined for myofibers and fibroblasts independently, but separate CSAs of the myooid cell types were not available since all of the myooid tissue was used for the biochemical assays. In light of this fact, we feel the normalization by total CSA provides some insight into the mechanisms of changing tissue contractile function. Protein specific Po, which normalized Po for differences in total MHC content [16], was calculated by dividing the specific Po by the ratio of MHC mass over total tissue mass. Two-tailed Student’s t-tests (INSTAT) were performed to compare adult and aged rat myooids at each time point after myooid formation.
The tissue from each group of 8 myooids was pooled, and the total mass was determined with a Mettler (model AE100) balance. MHC proteins were extracted from the myooids, soleus and gastrocnemius muscles, and 10T1/2 fibroblasts (American Type Culture Collection - ATCC, cultured according to the vendor’s instructions) by the method of Butler-Browne and Whalen [17]. The tissues, whether myooids, muscle, or cultured fibroblasts, were dissociated by hand in a ground-glass tissue homogenator. Four volumes of a solution of 0.3 M NaCl, 0.1 M NaH2PO4, 0.05 M Na2HPO4, 0.01 M sodium pyrophosphate, 1 mM MgCl2, 10 mM EDTA, and 1.4 mM 2-mercaptoethanol, adjusted to pH 6.5, were added to the tissue slurry, which was put on ice for 1 hour. This solution was spun down in a microcentrifuge, and the supernatant was added to 9 volumes of a solution of 40 mM sodium pyrophosphate and 50% glycerol, adjusted to pH 8.5. Solutions of extracted MHC proteins were stored at -20°C until separated electrophoretically.
A BCA Protein Assay Kit (Pierce # 23225) was used to determine the extracted MHC concentration for each myooid group, and the total MHC protein extracted was calculated by multiplying the MHC concentration by the total volume. A modification of the SDS-PAGE method of LaFromboise et al. [18] was used to separate the myosin isoforms. The separating gel consisted of 30 % glycerol, 28 % ddH2O, 25% stock separating buffer (1.5 M Tris (Bio-Rad # 161-0719), 4% SDS (Sigma # L-3771), pH adjusted to 6.8), 16.5 % stock acrylamide (T=30%, C=5%, Bio-Rad # 161-0154), 0.3 % ammonium persulfate (Sigma # A-3678) and 0.05 % TEMED (Bio-Rad # 161-0800). Glycerol, water, buffer and acrylamide were combined in a vacuum flask, mixed until only one liquid phase remained, and degassed for 10 minutes. Ammonium persulfate and TEMED were added, and then the solution was mixed and poured into a gel casting stand (PROTEAN II xi CELL, Bio-Rad). The cast gel solution was weighed down with ddH2O. Polymerization was complete in 1 to 2 hours. The water was decanted from the separating gel just before addition of the stacking gel. The stacking gel consisted of 65% ddH₂O, 25% stacking buffer (defined below), 10% stock acrylamide, 0.03% ammonium persulfate, and 0.07% TEMED. Stacking gel buffer consisted of 0.5 M Tris, and 4% SDS, pH adjusted to 6.8. Water, buffer, and acrylamide were combined, degassed for 10 minutes, ammonium persulfate and TEMED were added, and the solution was mixed and poured over the separating gel. Upper and lower running buffers were made by dilution of 10X stock buffer (Sigma # T7777).
Protein samples loaded in each lane were 100 µl in total volume. They were prepared with 50 µl Laemmli buffer (Bio-Rad # 161-0737) to which was added the extracted myosin solution, after which the total volume was brought up to 100 µl with a solution of 1 mM EDTA. Samples were boiled for 2 minutes, cooled, and loaded into the gel lanes. Electrophoresis was carried out at a constant 120 V for 24 hours, at 15°C. SDS-PAGE gels were fixed with Sigma fixing solution (F-7264) and stained with Brilliant Blue G-perchloric acid solution (Sigma B-8772) according to the manufacturer’s instructions. Proteins were densitometrically quantified using ImageQuanNT software. It was assumed that staining intensity was linear with protein concentration and that all MHC isoforms stained equally well with coomassie blue. MHC isoforms were identified by migration rate relative to MHC isoforms known to be present in control skeletal muscles.
Results
Myooids from adult rat muscle formed after ~18 days in culture, whereas those cultured from aged rats formed after ~28 days. All comparisons between the groups were made from the time of myooid formation. Although changes in cell phenotype with time in culture may confound comparisons from time of myooid formation, myooid formation and subsequent tissue remodeling had a greater influence on myooid properties than did time in culture based on functional data from this study as well as an earlier myooid time course study(20). For both adult and aged rat myooids, the diameter of the myooids decreased with time in culture, but the diameter decreased more rapidly for aged than for adult rat myooids (Figure 1).
Figure 1.Myooid diameter versus time in culture for adult and aged rat myooids.Each point represents the average diameter of 8 myooids + SEM. Statistically significant differences between the groups are indicated by (*) for the level of P < 0.05 and (***) for P < 0.001.
Figure 2.Myooid rheobase versus time in culture for adult and aged rat myooids.Rheobase was measured at 50% of Pt. Increased rheobase indicates decreased excitability with respect to stimulus amplitude. Each point represents the average rheobase of 8 myooids + SEM. Statistically significant differences between the groups are indicated by (*) for the level of P < 0.05, (**) for P < 0.01, and (***) for P < 0.001.
The rheobase for adult rat myooids did not change with time in culture (Figure 2). Initially, the rheobase for aged rat myooids was less than that for adult rat myooids (p < 0.05), but with time in culture the rheobase for the aged rat myooids increased until it was not different from that of the adult rat myooids. Thus, in terms of stimulus intensity, the aged rat myooids were initially more excitable than the adult rat myooids, but with time in culture they became less excitable. Chronaxie data were found to be linearly dependent on rheobase data and so are not reported and were not used for subsequent data analysis.
Figure 3.Myooid specific baseline force (sPb) versus time in culture for adult and aged rat myooids.Each point represents the mean sPb of 8 myooids + SEM. Statistically significant differences between the groups are indicated by (***) for P < 0.001.
Adult rat myooids had higher specific Pb (p < 0.05) than did aged rat myooids (Figure 3). The specific Pb did not change with time for aged rat myooids, while specific Pb increased with time for adult rat myooids. Adult and aged rat myooids had specific Pt and specific Po that were initially low, increased (p < 0.05) to reach peaks ~3-7 days after myooid formation, and then decreased with time (Figures 4‒5). Although at days 3 and 7 after myooid formation, aged rat myooids had specific Pt and specific Po greater (p < 0.05) than the values for adult rat myooids, the specific Pt and specific Po of the aged rat myooids decreased more rapidly than those of the adult rats with time so that by 24 days the values for the aged were not different from the values for adult rat myooids. Pt/Po ratios of the very old rat myooids were greater (p < 0.05) at days 1, 3, and 7 than Pt/Po ratios of adult rat myooids but decreased with time, while Pt/Po ratios of adult rat myooids increased with time (Figure 6). By 24 days, the values for the adult were higher than those of the very old rat myooids.
Figure 4.Myooid specific twitch force (sPt) versus time in culture for adult and aged rat myooids.Each point represents the mean sPt 8 myooids + SEM. Statistically significant differences between the groups are indicated by (***) for P < 0.001.
Figure 5.Myooid specific tetanic force (sPo) versus time in culture for adult and aged rat myooids.Each point represents the mean sPo of 8 myooids + SEM. Statistically significant differences between the groups are indicated by (*) for the level of P < 0.05 and (**) for P < 0.01.
Figure 6.Myooid twitch-tetanus ratio versus time in culture for adult and aged rat myooids.Each point represents the mean Pt/Po ratio of 8 myooids + SEM. Statistically significant differences between the groups are indicated by (**) for P < 0.01 and (***) for P < 0.001.
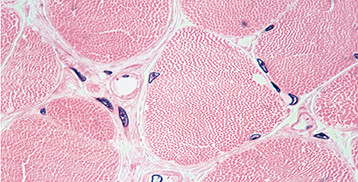
Myooids of both adult and aged rat origin expressed several MHC isoforms that corresponded to those found in cultured fibroblasts, as well as at least one skeletal muscle isoform (Figure 7). For adult and aged rat myooids, 5 bands of MHC were found. Of these, the four slowest-migrating were also found in fibroblast cultures. The fastest-migrating band was not found in cultures of fibroblasts, and co-migrated with skeletal muscle MHC IIa/x found in the hindlimb muscles of adult rats, indicating it could be one of these isoforms or a neonatal isoform that is known to migrate between these two isoforms [19]. Band four was 25+3.1% of the total MHC in myooids and band five was 35+5.8%. Skeletal muscle MHC was therefore at least 35% and at most 60% of the total MHC, with the balance of the MHC being isoforms expressed in fibroblasts. Percent of total myooid mass that was MHC did not trend for either group, but was greater for aged rat myooids (4.9+0.34%) than for adult rat myooids (4.2+0.25%). When myosin was extracted from whole soleus and gastrocnemius muscles of adult rats by the same method, the mass of MHC was 4.3% and 5.3% of the total mass respectively, indicating that myooids have total MHC content that is not different from that of control skeletal muscle. When specific Po was normalized by the amount of total myooid mass that was MHC, no differences remained in protein specific Po between adult and aged rat myooids except for the significant difference observed on day 3 (p < 0.05) (Figure 8).
Figure 7.SDS-PAGE gels stained with Coomassie blueLanes are extracted myosin heavy chain proteins from soleus muscle (Sol), adult rat myooid, gastrocnemeus muscle (Gas) and fibroblast culture (Fib). Arrows on the left side of the myooid lanes in Plate A indicate fibroblast isoforms of myosin heavy chain, while the arrows on the right indicate skeletal muscle myosin heavy chain, either IIa/x or neonatal isoforms. Myosin isoforms from predominantly fast-twitch (Gas) muscle and predominantly slow-twitch (Sol) muscle are compared with the MHC in the cultured myooids in plate B. The MHC IIa/IIx band constitutes 35% of the total MHC in the myooid.
Figure 8.Myooid protein specific tetanic force (psPo) versus time in culture for adult and aged rat myooids.Because all myooids are cultured at the same length (12 mm), protein specific force normalizes maximum tetanic forces by both cross-sectional area and MHC content. Each point represents the average contractility of 8 myooids + SEM. Statistically significant differences between the groups are indicated by (**) for P < 0.01.
Discussion
Although satellite cells are not the sole source of myoblastic cells in muscle regeneration [20], satellite cells are certainly the major source [4,21,22]. Based on the decreased number of satellite cells in skeletal muscles of old rats [10,23,24], the decreased proliferative capacity of satellite cells from muscles of old compared with young rats [2], and the decreased regenerative capacity of skeletal muscles in old compared with young rats [25,26], we hypothesized that the primary cultures of skeletal muscles from old rats would produce myooids, but that the myooids would have a lower success rate of formation, be smaller and generate lower specific forces. The observations of no difference in the success rate for the generation of myooids, >95%, the diameter of the myooids grown from primary cultures of skeletal muscles from old compared with the young rats, as well as the higher specific Pos (kN/m2 total myooid CSA) for the old than for young rat myooids at 4 and 8 days and the lack of any difference thereafter resulted in the rejection of the second part of the hypothesis. The old rat myooids generate specific force as well as, if not better than, the adult rat myooids and considerably better than neonatal rat myooids [7]. Some insight into the success of primary cultures of skeletal muscles of old rats is garnered from the transplantation of whole skeletal muscles among young and old rats of a highly inbred strain [27]. Muscles transplanted from limbs of young into young, or old into young had three-fold greater masses and forces than those transplanted old into old or young into old. Apparently, satellite cells from skeletal muscles of old animals when provided with a similarly optimal environment for replication as those of adult (young) animals, regenerate as well as the adult. That is, satellite cells from old rats transplanted into younger rats will regenerate muscle that has physiologic function as if the satellite cells were from young, not old, rats.
The null hypothesis that the contractile properties of adult and aged rat myooids were not different was not supported. Based upon this unexpected result, we hypothesize that the superior contractility of myooids engineered from muscles of aged animals arises from the tendency of satellite cells to preferentially express MHC isoforms of the muscle fiber with which they had been most closely associated, as has been shown in monolayer cultures of muscle cells [28,29] in which satellite cells associated with, for example, slow twitch fibers will, in culture, express slightly more adult slow twitch myosin isoform [29]. We hypothesize that this effect is reinforced with increasing age of the animal, and that muscle from older animals will have satellite cells with an increasingly persistent expression of adult myosin isoforms in culture, corresponding to the muscle fiber with which the satellite cell had been most closely associated. Nonetheless, the issue of satellite cell diversity remains controversial [30].
Thus, it appears that in the context of a transplant, the age of the recipient may dominate the resulting phenotype of the transplanted muscle, whereas in in vitro cell culture, it is the muscle phenotype with which the satellite cells were most closely associated while in the donor, and the age of the donor (the length of time of association with muscle of a specific phenotype) which dominates the resulting phenotype of the regenerated or newly formed muscle tissue in culture.
The diameter is the most easily obtained measure of the myooid growth and development [5-7] as it can be measured directly on a simple optical microscope with a calibrated reticle or a simple low-magnification digital image. The diameter provides some measure of function since over a range of diameters from 225 m to 775 m the specific force correlates with diameter with an R2 value of 0.804 [5]. Regardless of the laminin density, Dennis & Kosnik [5] reported that the diameter, and consequently the CSA of the myooids, declined linearly with time after the formation of the myooids. The diameter of both the old and the adult rat myooids in the present study and neonatal myooids in a previous study [7] have shown a similar, more or less linear, decrease with time after formation. Despite the accessibility of the measurement of diameter, the diameter does not provide an accurate measure of the proportion of the CSA composed of viable muscle tissue, because the diameter is strongly influenced by the thickness of the rim of fibroblasts that surrounds each myooid [5-7]. The fibroblast CSA was not measured in the present study, but the baseline force is highly correlated with the total fibroblast CSA (R2 = 0.74) [7]. Consequently, an estimate of the fibroblast composition can be made from the baseline force measurements. For the adult compared with the old rat myooids, the much larger, 3-fold to six-fold, normalized baseline forces, with little difference in diameters, suggests that the adult rat myooids had a much larger portion of the total CSA composed of fibroblasts. Compared with adult or old rat myooids, the approximately two-fold larger diameter of neonatal rat myooids from day 1 through day 17 results almost exclusively from the two-fold greater area of the myooid cross section composed of fibroblasts (~20% and 40%, respectively) [7]. Thus the proportion of the myooid composed of fibroblasts appears to be influenced by the age of the rats that provided the muscle tissue. The proportion of fibroblasts observed in the rat myooids was smallest in those from old, intermediate in those from adult and greatest in those from neonatal rats.
The percentage of MHC content of the total myooid mass is not different from the value of 4-5 % reported for control skeletal muscles. Despite the similarity in the percentage, unlike control skeletal muscles, wherein 100% of the MHC is skeletal muscle MHC, the MHC content of myooids is composed of both muscle MHC isoforms, and non-muscle isoforms normally found in fibroblast cultures. The one skeletal muscle isoform of MHC found in myooids appears to be either neonatal, IIa, or IIx. The functional data suggest that this band represents the neonatal isoform, since Pt/Po. ratios of myooids are ~0.6, indicative of developmental isoforms, while adult isoforms yield Pt/Po ratios of ~0.2 [6]. In addition, myooids may contain embryonic MHC, which can co-migrate with the fastest-migrating of the fibroblast MHC [18]. Our estimate that of the total MHC expressed by myooids, only 35% to 60% is skeletal muscle MHC isoforms, translates to ~2% of the myooid mass composed of MHC. These data support the hypothesis that myooids have much less skeletal muscle MHC per unit mass than skeletal muscles.
Compared with the specific force of ~ 250 kN/m2 generated by control hind limb muscles of adult rats [25,31], those of neonatal rats [31] generate ~65 kN/m2 and those of aged rats(3) ~210 kN/m2. Since myooids contain only about half of the skeletal muscle MHC of control adult skeletal muscles and the skeletal muscle MHC they contain generates only a quarter of the specific force of the adult isoforms, a reasonable prediction for specific force is ~12% of the value for control adult skeletal muscle. Although this is much greater than the 1-3% generated by myooids in this study, the MHC composition and isoforms observed in the myooids explain a considerable portion of the discrepancy between the specific force development of myooids and that of control adult skeletal muscles. The six-fold difference that remains is likely attributable to the general disorganization of the myofibrillar proteins and absence of well-organized sarcomeric arrays observed in electron micrographs [5,6].
The myooids undergo a considerable amount of remodeling with the time after formation. The remodeling is reflected grossly by the decrease in the total diameter of the myooid(8; 20) and particularly in the present study, concurrent with a significant increase in specific force. During the first few days after myooid formation, on slightly different time scales, the specific force of both adult and old myooids increased 2.6-fold when myooid diameter decreased by 30%. The only interpretation is that the myofibrillar apparatus within the myooids underwent a restructuring that enhanced force generation at a time when the total CSA of the myooid decreased. The phenomenon was observed with normalization of the force by either total CSA or MHC protein CSA, although for the old rat myooids a 40% decrease in MHC protein specific force occurred between day 3 and day 8, indicating both positive and negative remodeling of the old rat myooids. Such an early remodeling was not observed in previous studies of myooids, but over a 40 day culture “life span” the specific force of neonatal rat myooids normalized by viable muscle CSA (total CSA minus fibroblast CSA) increased from 0.25 kN/m2 to 4.0 kN/m2. The 16-fold increase in specific force of the neonatal rat myooids occurred simultaneously with a decrease in the diameter from 0.90 mm to 0.34 mm, a decrease of 62% [7]. For the adult rat myooids in the present study, during the first 25 days after myooid formation, the baseline force/total CSA increased from 1.8 kN/m2 to 6.9 kN/m2 strongly indicative of an ~4-fold increase in the area composed of fibroblasts[7]. Interestingly, for the adult rat myooids, during the first 8 days, the specific force was increasing despite a decrease in the diameter coupled with an increase in the percentage of the fibroblast CSA.
In conclusion, we find that myogenic precursor cells harvested from the limb muscles of aged rats retain significant potential for myogenesis in culture when compared with myogenic precursor cells harvested from adult or neonatal rats. The excitability and contractility of engineered muscle from aged mammalian tissues is equivalent or superior to that of muscle engineered from either adult or neonatal tissue sources. Although myooids from adult and aged rats had as much total MHC protein as did control skeletal muscle, only ~35-60% of it consisted of skeletal muscle isoforms, the balance being isoforms found in fibroblast cultures. MHC data explained much of the functional deficit of myooids compared to adult skeletal muscle controls. Ultimately, the ability of any of these tissue sources to yield cells that can self-organize into fully adult phenotype muscle organs in vitro is yet to be demonstrated, but our current data support the conclusion that self-organizing functional skeletal muscle tissue can be engineered from myogenic precursor cells harvested from aged mammals (rats), which are thought to be equivalent to ~90 year-old humans.
Acknowledgements
This work was supported by grants NIH #2 PO1 AG 10821, and NIA #AG00114-17
Statement of Conflict of Interest
The authors declare no financial interest and no conflicts of interest related to this research, perhaps fewer than primarily academically-appointed scientists, as this research has no bearing whatsoever on current commercial activities, nor matters of promotion, reappointment, tenure, salary, title, funded or planned research proposals (grants), or professional standing with any academic institution in any way.
References
- Allbrook D. B., Han M. F., Hellmuth A. E.. Population of Muscle Satellite Cells in Relation to Age and Mitotic Activity. Pathology. 1971; 3(3)DOI
- Schultz Edward, Lipton Bruce H.. Skeletal muscle satellite cells: Changes in proliferation potential as a function of age. Mechanisms of Ageing and Development. 1982; 20(4)DOI
- Snow MH. Effects of Aging on Satellite Cells in Skeletal-Muscles of Mice and Rats.. Cell and Tissue Research. 1977; 185:399-408.
- Snow Mikel H.. Myogenic cell formation in regenerating rat skeletal muscle injured by mincing II. An autoradiographic study. The Anatomical Record. 1977; 188(2)DOI
- DENNIS ROBERT G., KOSNIK, II PAUL E.. EXCITABILITY AND ISOMETRIC CONTRACTILE PROPERTIES OF MAMMALIAN SKELETAL MUSCLE CONSTRUCTS ENGINEERED IN VITRO. In Vitro Cellular & Developmental Biology - Animal. 2000; 36(5)DOI
- Dennis Robert G., Kosnik Paul E., Gilbert Mark E., Faulkner John A.. Excitability and contractility of skeletal muscle engineered from primary cultures and cell lines. American Journal of Physiology-Cell Physiology. 2001; 280(2)DOI
- Kosnik Paul E., Faulkner John A., Dennis Robert G.. Functional Development of Engineered Skeletal Muscle from Adult and Neonatal Rats. Tissue Engineering. 2001; 7(5)DOI
- Dennis RG, Kosnik PE. Mesenchymal Cell Culture: Instrumentation and Methods for Evaluating Engineered Muscle.. Methods in Tissue Engineering. 2002;307-316. DOI
- Decary S., Mouly V., Hamida C. Ben, Sautet A., Barbet J. P., Butler-Browne G. S.. Replicative Potential and Telomere Length in Human Skeletal Muscle: Implications for Satellite Cell-Mediated Gene Therapy. Human Gene Therapy. 1997; 8(12)DOI
- Gibson Marcia C., Schultz Edward. Age-related differences in absolute numbers of skeletal muscle satellite cells. Muscle & Nerve. 1983; 6(8)DOI
- Snow MH. Metabolic-Activity During Degenerative and Early Regenerative Stages of Minced Skeletal-Muscle. Anatomical Record. 1973; 176:185-203.
- Kosnik PE, Dennis RG. Mesenchymal Cell Culture: Functional Mammalian Skeletal Muscle Constructs. Harcourt, Academic Press: San Diego; 2002. DOI
- Dennis RG. Measurement of Pulse Propagation in Single Permeabilized Muscle Fibers by Optical Diffraction. 1996.
- Kosnik PE. Contractile Properties of Engineered Skeletal Muscle. 2000.
- Minns H. G.. A voltage-controlled force generator for calibrating sensitive transducers. Journal of Applied Physiology. 1971; 30(6)DOI
- Taylor J. A., Kandarian S. C.. Advantage of normalizing force production to myofibrillar protein in skeletal muscle cross-sectional area. Journal of Applied Physiology. 1994; 76(2)DOI
- Butler-Browne Gillian S., Whalen Robert G.. Myosin isozyme transitions occurring during the postnatal development of the rat soleus muscle. Developmental Biology. 1984; 102(2)DOI
- LaFramboise William A., Daood Monica J., Guthrie Robert D., Moretti Paolo, Schiaffino Stefano, Ontell Marcia. Electrophoretic separation and immunological identification of type 2X myosin heavy chain in rat skeletal muscle. Biochimica et Biophysica Acta (BBA) - General Subjects. 1990; 1035(1)DOI
- Naumann Karin, Pette Dirk. Effects of chronic stimulation with different impulse patterns on the expression of myosin isoforms in rat myotube cultures. Differentiation. 1994; 55(3)DOI
- Ferrari Giuliana, Cusella– Gabriella, Angelis De, Coletta Marcello, Paolucci Egle, Stornaiuolo Anna, Cossu Giulio, Mavilio Fulvio. Muscle Regeneration by Bone Marrow-Derived Myogenic Progenitors. Science. 1998; 279(5356)DOI
- Mauro Alexander. SATELLITE CELL OF SKELETAL MUSCLE FIBERS. The Journal of Biophysical and Biochemical Cytology. 1961; 9(2)DOI
- Snow Mikel H.. Myogenic cell formation in regenerating rat skeletal muscle injured by mincing II. An autoradiographic study. The Anatomical Record. 1977; 188(2)DOI
- Snow MikelH.. The effects of aging on satellite cells in skeletal muscles of mice and rats. Cell and Tissue Research. 1977; 185(3)DOI
- Snow MH. Myosatellite Cells in Mature and Senile Skeletal-Muscle of Mouse. Anatomical Record. 1977; 187:718-719.
- Carlson Bruce M., Faulkner John A.. Reinnervation of long-term denervated rat muscle freely grafted into an innervated limb. Experimental Neurology. 1988; 102(1)DOI
- Gutmann Ernest, Carlson Bruce M.. Regeneration and transplantation of muscles in old rats and between young and old rats. Life Sciences. 1976; 18(1)DOI
- Carlson B. M., Faulkner J. A.. Muscle transplantation between young and old rats: age of host determines recovery. American Journal of Physiology-Cell Physiology. 1989; 256(6)DOI
- Dusterhoft S, Yablonkareuveni Z, Pette D. Myosin Expression in Satellite Cell-Cultures from Fast and Slow Twitch Muscles of the Rat. Journal of Muscle Research and Cell Motility. 1991; 12:71-72.
- Düsterhöft Sabine, Pette Dirk. Satellite cells from slow rat muscle express slow myosin under appropriate culture conditions. Differentiation. 1993; 53(1)DOI
- Dusterhöft Sabine, Yablonka-Reuveni Zipora, Pette Dirk. Characterization of myosin isoforms in satellite cell cultures from adult rat diaphragm, soleus and tibialis anterior muscles. Differentiation. 1990; 45(3)DOI
- Close R.. Dynamic properties of fast and slow skeletal muscles of the rat during development. The Journal of Physiology. 1964; 173(1)DOI